CRISPR gene editing represents a groundbreaking leap in modern science, enabling precise alterations to DNA that could revolutionize treatment for diseases like sickle cell disease. As researchers harness the power of this gene editing technology, they encounter not only the potential to cure debilitating ailments but also a host of ethical dilemmas, steeped in debates about CRISPR ethics and health equity. The promise of gene therapy through CRISPR raises compelling questions: Should we employ these tools to edit human traits, and who gets to make those choices? While the ability to edit genes presents opportunities for unprecedented healing, it also necessitates a cautious examination of the moral implications tied to such power. Striking a balance between innovation and ethical responsibility is vital as we navigate the future of genetic modification.
The advent of gene modification techniques, especially through methods like CRISPR technology, is reshaping the landscape of medical science in extraordinary ways. This sophisticated approach allows scientists to manipulate genetic material, providing potential routes for addressing genetic conditions, including those that affect the quality of life, like sickle cell anemia. However, as humanity stands on the cusp of a new era in genetic intervention, discussions surrounding the responsibilities and repercussions of such advancements become increasingly crucial. The implications of gene editing extend beyond mere medical treatments, influencing ethical considerations and raising important questions about health equity and access to these life-changing technologies. As the dialogue around gene therapies evolves, it becomes essential to consider not just the scientific capabilities but also the socio-ethical landscape in which these innovations will operate.
Understanding CRISPR Technology and Its Applications
CRISPR gene editing technology revolutionizes the way scientists approach genetic diseases. By allowing precise alterations in the DNA of living organisms, CRISPR holds significant promise for treating conditions like sickle cell disease, which previously left little hope for effective treatment. This biotechnology enables not only the editing of somatic genes to alleviate symptoms in patients but also germline editing, which could potentially eradicate hereditary diseases from future generations. This dual capability of CRISPR presents a pivotal moment in medical science, opening doors to cures that could redefine health outcomes for millions.
However, while the applications of CRISPR gene editing are promising, they raise intricate ethical questions. The ability to edit genes does not just change the lives of those currently suffering; it also has profound implications for how we understand human variation. As we tread deeper into the world of genetic manipulation, society must assess who benefits from these advancements and at what cost. The possibility of making genetic decisions on behalf of future generations complicates the landscape of personal choice, ethical responsibility, and the very definition of what it means to be human.
Ethical Implications Surrounding Gene Editing
The introduction of CRISPR technology into medical practice introduces numerous ethical dilemmas. Key amongst these is the question of whether we have the right to alter human genetics, especially in cases where disabilities, like Down syndrome, are involved. The philosophical debate about whether to ‘fix’ certain human conditions touches on deep societal values and definitions of normalcy. This prompts critical reflections on inclusivity and acceptance within our communities, bringing to light the potential for discrimination against those who might be categorized as ‘differently-abled.’ As Dr. Neal Baer noted during a recent talk, determining who gets to make these decisions is a pressing concern that society must confront.
Moreover, the financial implications of implementing CRISPR gene editing treatments cannot be overlooked. The estimated cost of curing diseases, like sickle cell disease, at around $2 million raises questions about access and health equity. As advancements in gene therapy emerge, the disparity between those who can afford cutting-edge treatments and those who cannot becomes starker. This reality fuels discussions around health justice, pushing for a future where medical innovations do not exacerbate existing inequalities. The ethical responsibility lies in ensuring that gene editing technologies extend benefits to all, not just those who fall within socioeconomic advantages.
Health Equity and Access to Gene Therapy
The emergence of gene editing technologies like CRISPR holds the potential to transform healthcare, particularly for underserved populations faces chronic diseases such as sickle cell disease. However, the high costs associated with advanced gene therapies introduce significant barriers to access. This financial divide raises critical questions about fairness in healthcare, as those who cannot afford expensive treatments are left without options. Advocates for health equity stress the importance of developing policies that ensure equitable access to these groundbreaking therapies, emphasizing that advancements should benefit all, regardless of economic status.
Moreover, to achieve health equity, it is vital to address both the ethical considerations surrounding gene editing and the systemic issues contributing to healthcare disparities. The dialogue around health justice not only calls for fair distribution of resources but also emphasizes the need for inclusive discussions about the future of medical innovations. Engaging diverse communities in conversations about the implications of gene therapy can help demystify the technology and foster an environment where ethical considerations are at the forefront of scientific advancement.
The Future of Genetic Modification and Societal Impact
As gene editing technologies advance, the future holds exciting yet daunting possibilities. CRISPR enables precision edits that could eradicate inherited conditions, fundamentally altering our approach to medicine. Yet, the societal implications of such technologies are complex. As noted by experts, the ability to manipulate genetics comes with a responsibility to consider the long-term effects on our species. The normalization of genetic editing might lead to societal pressure to enhance genetic traits, raising ethical concerns about the implications for human diversity and individuality.
Furthermore, as seen in discussions surrounding potential military applications of gene editing, the consequences extend beyond health into realms of bioethics and national security. The concern about genetically modified soldiers, for instance, illustrates the potential for misuse of gene editing technology. This reality calls for stringent ethical oversight and regulatory frameworks to guide the responsible application of gene editing. Balancing innovation with ethical considerations is crucial as society navigates the uncharted territory of genetic advancement.
CRISPR Ethics: Navigating the Challenges Ahead
The ethics of CRISPR gene editing present a multifaceted challenge for researchers, clinicians, and policymakers. As the technology evolves, so too must our understanding of its ethical boundaries. Who decides what constitutes a desirable genetic trait? The historical context of eugenics looms large, reminding us of the dangers inherent in making genetic modifications based on subjective criteria. Discussions during recent talks, including the insights shared by Dr. Baer and Brendel, highlight the complexity of these ethical discussions and the need for inclusive dialogues that consider multiple perspectives.
Moreover, the urgency to establish ethical guidelines cannot be overstated. As CRISPR continues to develop rapidly, the potential for controversial applications, such as germline editing, requires robust discussions among ethicists, scientists, and the public. Establishing ethical frameworks that prioritize human rights and dignity is essential to mitigate the risks associated with genetic manipulation. These discussions are not only necessary but imperative as we navigate the profound capabilities technology offers.
Challenges and Innovations in Gene Editing
Innovations in gene editing, particularly through CRISPR, are progressing at an unprecedented rate, promising breakthrough treatments for various genetic disorders. Yet, there remains a substantial gap between the science itself and its practical application in clinical settings. The challenges surrounding ethical implications, costs, and equitable access remain obstacles to widespread adoption of these technologies. Researchers are increasingly confronted with the duty to evaluate the ramifications of their work beyond the laboratory, focusing on how advances can translate into real-world benefits for patients.
Moreover, ambition within the biotechnological sphere must be matched by caution. While the potential for cures is alluring, the question of unintended consequences looms large. As noted by Baer during discussions, gene alteration can lead to effects that extend far beyond initial expectations. Stakeholders must prioritize thorough investigations into the long-term impacts of gene editing, ensuring that innovations advance human health without compromising ethical standards.
The Role of Public Perception in Gene Editing
Public perception plays a crucial role in the evolution and acceptance of gene editing technologies. As people become more aware of CRISPR and its potential, it is essential to foster informed conversations about its applications and implications. Misinformation can lead to public fear or skepticism about genetic technologies. Therefore, education and transparency around the science of gene editing, as well as the ethical conversations surrounding it, are critical for cultivating a well-informed public that can engage in meaningful dialogues.
Furthermore, the media also plays a significant role in shaping public narratives about gene editing. As seen in shows that dramatize medical ethics, storytelling can serve to highlight the complexities and human stories behind scientific advancements. Balancing sensationalism with factual integrity is essential in promoting an accurate understanding of CRISPR technology and its ethical ramifications. Engaging a diverse range of voices in these narratives will help bridge the gap between scientific communities and the broader society, ultimately guiding the future of gene editing in a responsible and equitable manner.
Innovating for Health Justice in Gene Therapy
As we advance in the field of gene therapy, innovation must prioritize health justice to ensure equitable access for all segments of the population. The significant costs associated with break-through treatments like those enabled by CRISPR often leave marginalized communities at a disadvantage. Addressing health equity requires critical evaluation of socioeconomic factors influencing access to gene therapies, alongside the establishment of policies aimed at narrowing these gaps. Incorporating diverse voices into discussions surrounding these innovations can lead to more comprehensive and just approaches to healthcare.
Additionally, fostering collaboration between various stakeholders—scientists, ethicists, policymakers, and community leaders—can pave the way for a more inclusive approach to gene therapy. By prioritizing voices from affected communities, the healthcare ecosystem can better understand the real-life implications of gene editing technologies. To realize the full potential of CRISPR in curing diseases while promoting health equity, the focus must remain on integrating fairness into the fabric of medical advancements.
Regulation and Oversight of CRISPR Technology
As CRISPR gene editing technology advances, the need for stringent regulation and oversight becomes increasingly crucial. Without comprehensive guidelines, the risks of unethical applications and potential misuse loom large. The responsibility falls on governments, ethical boards, and scientific institutions to establish clear frameworks that govern the use of gene editing technologies. This regulation should not only focus on the technology’s application in clinical settings but also encompass research and experimental phases.
The international landscape for regulation is fragmented, making it imperative for global conversations about the direction of gene editing. As Baer highlights, the unchecked potential for gene manipulation in places where oversight is lacking raises alarms about ethical responsibility. International cooperation and adherence to shared ethical standards are vital in ensuring that CRISPR technology advances human health while significantly reducing risks associated with misuse and unintended consequences.
Frequently Asked Questions
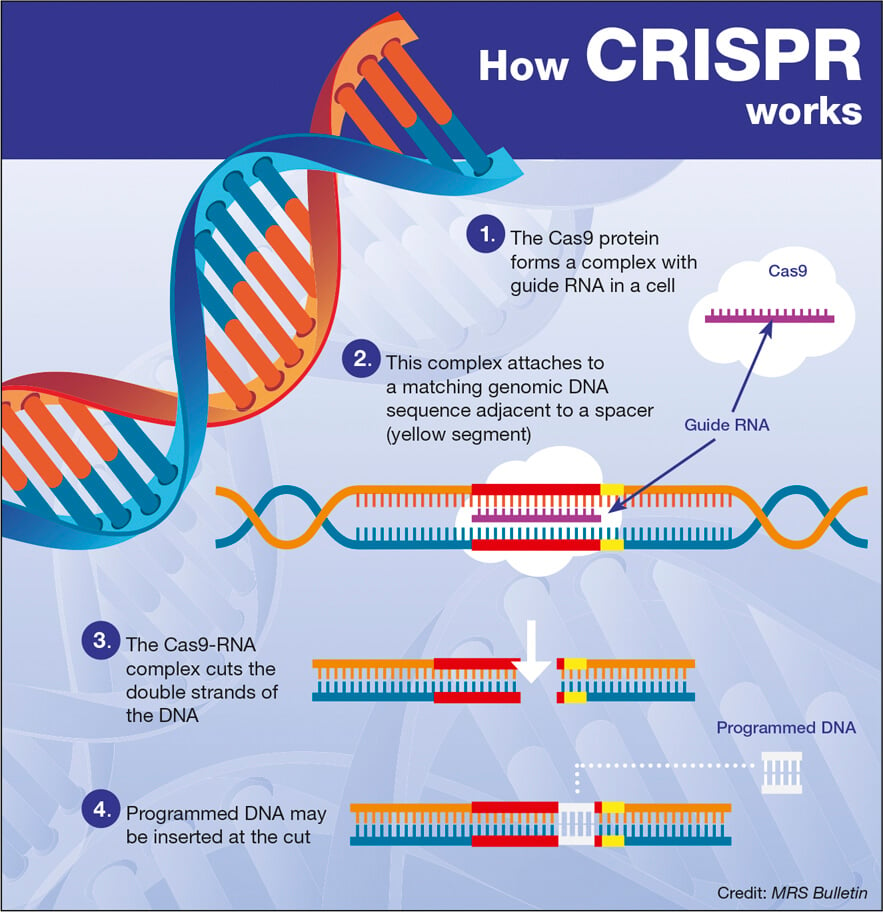
What is CRISPR gene editing and how does it work?
CRISPR gene editing is a revolutionary gene editing technology that allows scientists to modify DNA within living organisms. It utilizes a protein called Cas9, which acts as a pair of molecular scissors to cut DNA at specific sites. This enables precise edits, such as removing or replacing faulty genes. The technology holds promise for treating genetic diseases, including sickle cell disease, by correcting the underlying genetic faults.
What ethical considerations surround CRISPR gene editing?
The use of CRISPR gene editing raises significant ethical questions, including the morality of altering human genes, particularly in germline editing, which affects future generations. Discussions often focus on whether it is appropriate to edit genes that do not cause severe health issues, such as altering traits linked to conditions like Down syndrome. There are concerns about who decides which traits to modify and the implications for diversity and health equity.
Can CRISPR be used in gene therapy for sickle cell disease?
Yes, CRISPR gene editing has been successfully applied in gene therapy for sickle cell disease. Researchers have been able to modify somatic cells to remove the genes that cause sickle cell anemia, effectively curing affected individuals. However, the high cost of these treatments, often around $2.2 million, raises questions about access and health equity for those in different socioeconomic situations.
How does CRISPR technology relate to health equity?
CRISPR technology has the potential to transform medicine by providing cures for genetic diseases. However, it also poses challenges to health equity. As advanced treatments become available, there is a concern that they may disproportionately benefit wealthier populations, leaving lower-income individuals at a disadvantage. Ensuring fair access to CRISPR gene editing technologies is crucial for advancing health equity.
What potential risks are associated with CRISPR gene editing?
While CRISPR gene editing holds great potential, it also carries risks such as unforeseen genetic changes and unintended consequences. For example, editing genes that regulate cholesterol can affect other biological processes, leading to complications. Additionally, there are concerns about the lack of regulation in some countries, which could result in misuse or harmful applications of the technology.
Should CRISPR gene editing be used to enhance human traits?
The use of CRISPR gene editing for non-therapeutic enhancements raises profound ethical dilemmas. Many experts argue that modifying traits such as intelligence or physical characteristics crosses a moral line, as it could alter the fabric of human diversity. The debate continues over who should make these decisions and the impact on societal norms.
What role does oversight play in CRISPR gene editing?
Oversight is crucial in the field of CRISPR gene editing to prevent unethical practices and ensure safety. While regulations exist in many countries preventing germline editing and cloning, enforcement can vary globally. Ongoing discussions emphasize the need for comprehensive regulations and monitoring to ensure responsible use of gene editing technologies.
What is the relationship between CRISPR and genetic diseases?
CRISPR has a transformative potential for treating genetic diseases by allowing precise editing of genes associated with these conditions. For example, it has shown promise in curing sickle cell disease by directly targeting the responsible genes. This technological advancement could revolutionize the management of various hereditary conditions.
| Key Points | Description |
|---|---|
| CRISPR Technology | CRISPR allows editing of both somatic and germline genes, potentially curing genetic diseases. |
| Ethical Concerns | Manipulation may raise questions about the right to change human traits and health equity. |
| Cost of Treatments | CRISPR-based cures can be extremely expensive, leading to fairness issues. |
| Health Justice | Innovation in gene editing must consider implications for health equity and justice. |
| Parental Decisions | The decision to modify children genetically raises ethical issues regarding parental choice. |
| Oversight Issues | Lack of global consensus on monitoring gene editing practices can lead to unethical applications. |
| Unintended Consequences | Gene editing can have unexpected effects due to complex interactions within genetic systems. |
Summary
CRISPR gene editing presents a revolutionary breakthrough in the field of genetics, offering potential cures for debilitating diseases like sickle cell anemia. However, as highlighted in recent discussions, this powerful technology brings troubling ethical questions to the forefront. The ability to change human genetics raises critical concerns about parental decision-making, accessibility to treatments, and the risks of unintended consequences. Thus, while CRISPR offers promising solutions, it is essential to navigate these complex challenges to ensure ethical and equitable access to genetic advancements.