In the quest to combat Alzheimer’s Disease, the discovery of TIM-3 as a crucial immune checkpoint molecule opens new avenues for innovative treatments. This research highlights how TIM-3 therapy can potentially bolster cognitive functions by allowing microglia to effectively target and clear amyloid plaques from the brain. By inhibiting TIM-3, scientists found a way to enhance the ability of these brain immune cells, thus improving memory in laboratory mice with Alzheimer’s. The implications for Alzheimer’s treatment are significant, especially in considering the role of immune system strategies previously utilized in cancer therapies. As TIM-3 gains attention, future investigations could pioneer a transformative approach to managing this devastating disease associated with cognitive decline and memory loss.
Exploring the relationship between the TIM-3 molecule and Alzheimer’s Disease reveals an exciting intersection of immune regulation and neurobiology. Known for its role in the immune checkpoint mechanisms, TIM-3 has emerged as a key player in the pathology of Alzheimer’s by impeding microglial activity, which is essential for clearing harmful brain protein aggregates. This presents a dual challenge for Alzheimer’s treatment, as effectively modulating TIM-3 could enhance the brain’s ability to combat cognitive deterioration linked with neurodegenerative diseases. By targeting this checkpoint molecule, researchers are seeking to untap the immune response to facilitate the clearance of neurotoxic plaques, potentially reversing memory impairment associated with Alzheimer’s. The continued study of TIM-3 could reshape therapeutic strategies aimed at improving the longevity and quality of life for those affected by Alzheimer’s.
Understanding TIM-3 and Its Role in Alzheimer’s Disease
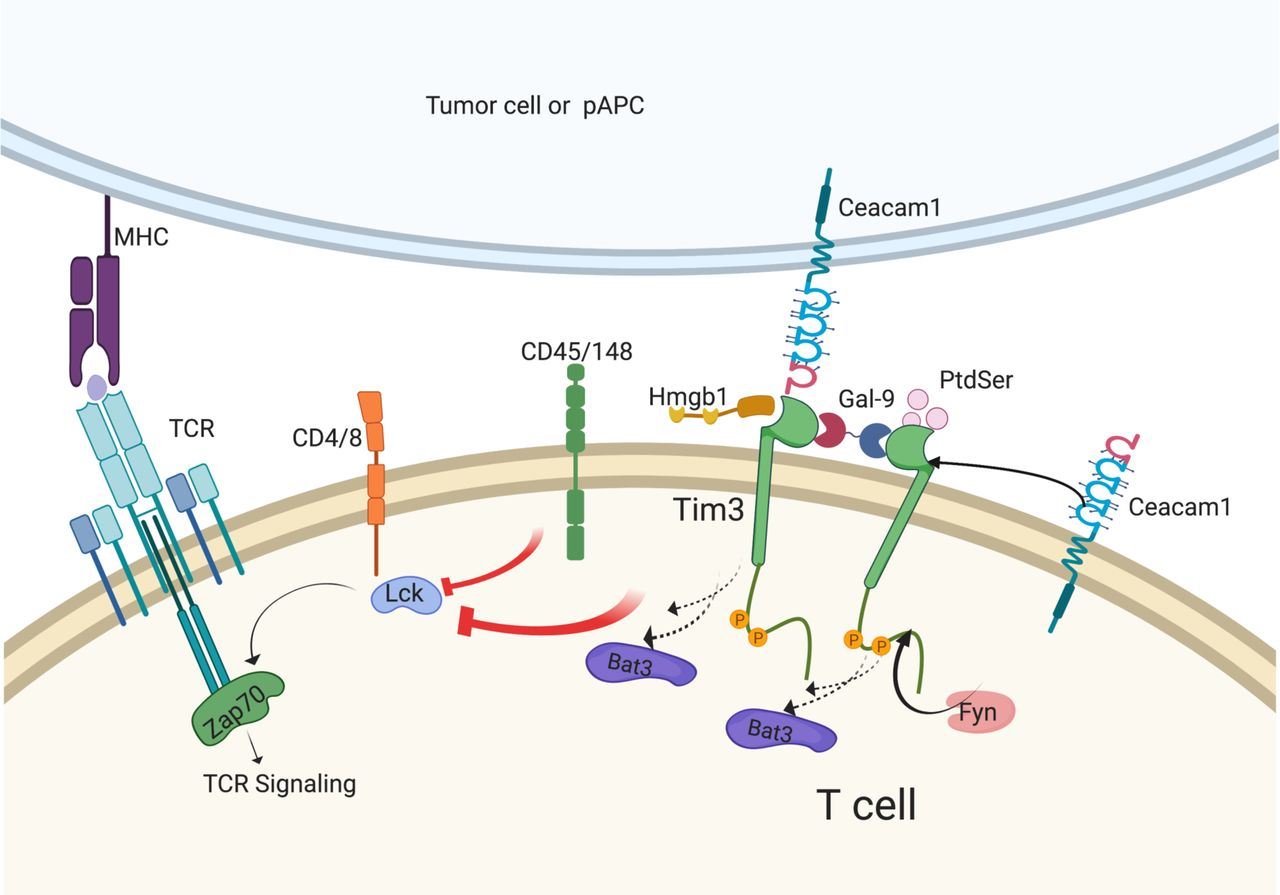
TIM-3 is a checkpoint molecule that has garnered significant attention in the context of Alzheimer’s disease (AD). This molecule plays a crucial role in regulating the immune response of microglia, the brain’s resident immune cells that are essential for maintaining cognitive function. By inhibiting the activation of microglia, TIM-3 prevents these cells from effectively clearing amyloid plaques, which are characteristic of Alzheimer’s pathology. The expression of TIM-3 in microglia increases with age and is particularly elevated in individuals with Alzheimer’s, demonstrating its correlation with the disease’s progression.
The research highlights the detrimental impact of TIM-3 on microglial functioning. Under normal circumstances, microglia engage in synaptic pruning and the clearance of extracellular debris. However, in the presence of elevated TIM-3, these cells become homeostatic, leading to the accumulation of neurotoxic plaques that impair cognitive function. Understanding the mechanisms that underlie TIM-3’s regulation of microglial activity represents a significant step towards developing effective therapies for Alzheimer’s disease.
Frequently Asked Questions
What is TIM-3 and how is it related to Alzheimer’s Disease?
TIM-3, or T-cell immunoglobulin and mucin-domain containing-3, is an immune checkpoint molecule that plays a significant role in regulating immune responses in the brain. In the context of Alzheimer’s Disease, TIM-3 is found to inhibit microglia from clearing amyloid plaques, which are damaging to cognitive function. This accumulation of plaques is associated with the progression of Alzheimer’s, making TIM-3 a critical target for potential therapies.
How does TIM-3 therapy improve cognitive function in Alzheimer’s models?
TIM-3 therapy aims to silence the TIM-3 checkpoint molecule in microglia, allowing these brain immune cells to effectively eliminate amyloid plaques associated with Alzheimer’s Disease. Studies have shown that deleting TIM-3 in mouse models leads to the clearance of plaques and an improvement in memory and cognitive function, indicating a promising avenue for treating Alzheimer’s.
What role do microglia play in Alzheimer’s disease and how does TIM-3 affect them?
Microglia are the immune cells of the brain responsible for clearing debris and maintaining synaptic health. In Alzheimer’s Disease, the expression of TIM-3 on microglia prevents them from attacking and removing amyloid plaques. This inhibition results in unhealthy plaque accumulation, which is detrimental to cognitive function. By blocking TIM-3, microglia can resume their cleaning functions, potentially alleviating Alzheimer’s symptoms.
What research supports the link between TIM-3 and late-onset Alzheimer’s Disease?
Recent studies, including a genome-wide association study, have identified TIM-3 as a genetic risk factor for late-onset Alzheimer’s Disease, which accounts for 90-95% of cases. Research has demonstrated that polymorphisms in the TIM-3 gene contribute to increased expression on microglia, impairing their ability to clear harmful plaques, thereby linking TIM-3 directly to the disease’s progression.
What are the potential next steps for TIM-3 therapy in Alzheimer’s treatment?
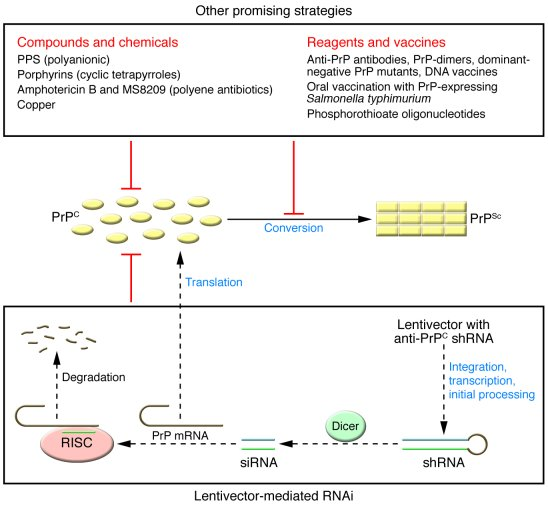
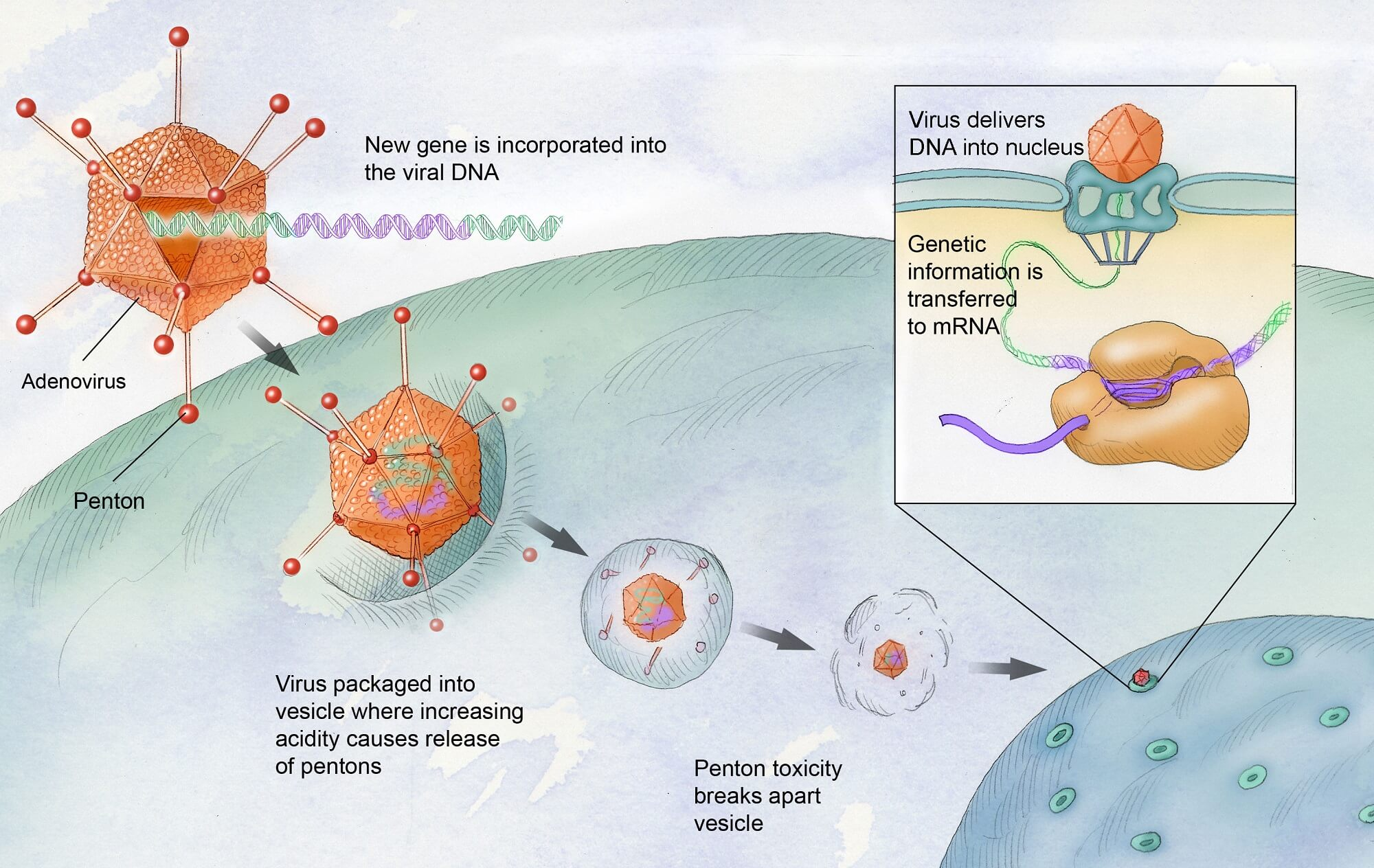
Following preliminary successes in animal models, the next steps for TIM-3 therapy in Alzheimer’s treatment involve testing human anti-TIM-3 antibodies in mouse models that mimic human Alzheimer’s pathology. This research aims to determine if inhibiting TIM-3 can effectively halt plaque development and improve cognitive function in humans, potentially leading to clinical trials.
How does TIM-3 therapy compare to traditional Alzheimer’s treatments?
Unlike traditional Alzheimer’s treatments that often focus on amyloid beta reduction, TIM-3 therapy targets the immune response by enhancing microglial function. Traditional drugs have shown limited success, whereas TIM-3 therapy could represent a novel approach by reinstating the brain’s ability to clear harmful plaques, thus potentially offering significant improvements in cognitive health.
What are the implications of TIM-3’s role in immune checkpoints for Alzheimer’s disease research?
The role of TIM-3 as an immune checkpoint molecule underscores a critical intersection between neuroinflammation and Alzheimer’s pathology. Understanding how TIM-3 operates may unlock new pathways for therapeutic interventions, not only for Alzheimer’s but also for other neurodegenerative diseases where immune response plays a vital role.
| Key Point | Description |
|---|---|
| TIM-3’s Role in Alzheimer’s Disease | TIM-3 is an immune checkpoint molecule that inhibits microglial activity, preventing them from clearing amyloid plaques in the brain, leading to cognitive decline. |
| Impact of TIM-3 Deletion | Genetically deleting the TIM-3 gene in mice allows microglia to clear plaques, leading to improved memory and cognitive function. |
| Late-Onset Alzheimer’s Disease | 90-95% of Alzheimer’s cases are late-onset, where genetic factors, including TIM-3, play a significant role. |
| Therapeutic Potential | Using anti-TIM-3 therapy could potentially promote plaque clearance and improve cognitive function in Alzheimer’s patients. |
| Complexity of Alzheimer’s Mechanism | Alzheimer’s disease involves complex interactions between immune response and brain health, with TIM-3 being at the center of this process. |
Summary
TIM-3 and Alzheimer’s Disease represent a significant intersection of immunology and neurodegeneration, highlighting the potential for existing cancer therapies to address neurodegenerative conditions. By understanding the role of TIM-3 in inhibiting microglial clearance of amyloid plaques, researchers have opened new avenues for treating late-onset Alzheimer’s disease. The deletion of TIM-3 in laboratory mice demonstrated promise by improving cognitive functions, paving the way for potential therapies that could harness this mechanism in human patients. As research continues, the hopeful application of anti-TIM-3 antibodies could offer a novel approach in the fight against Alzheimer’s, suggesting that innovative strategies may finally lead to successful interventions in this challenging area of medicine.