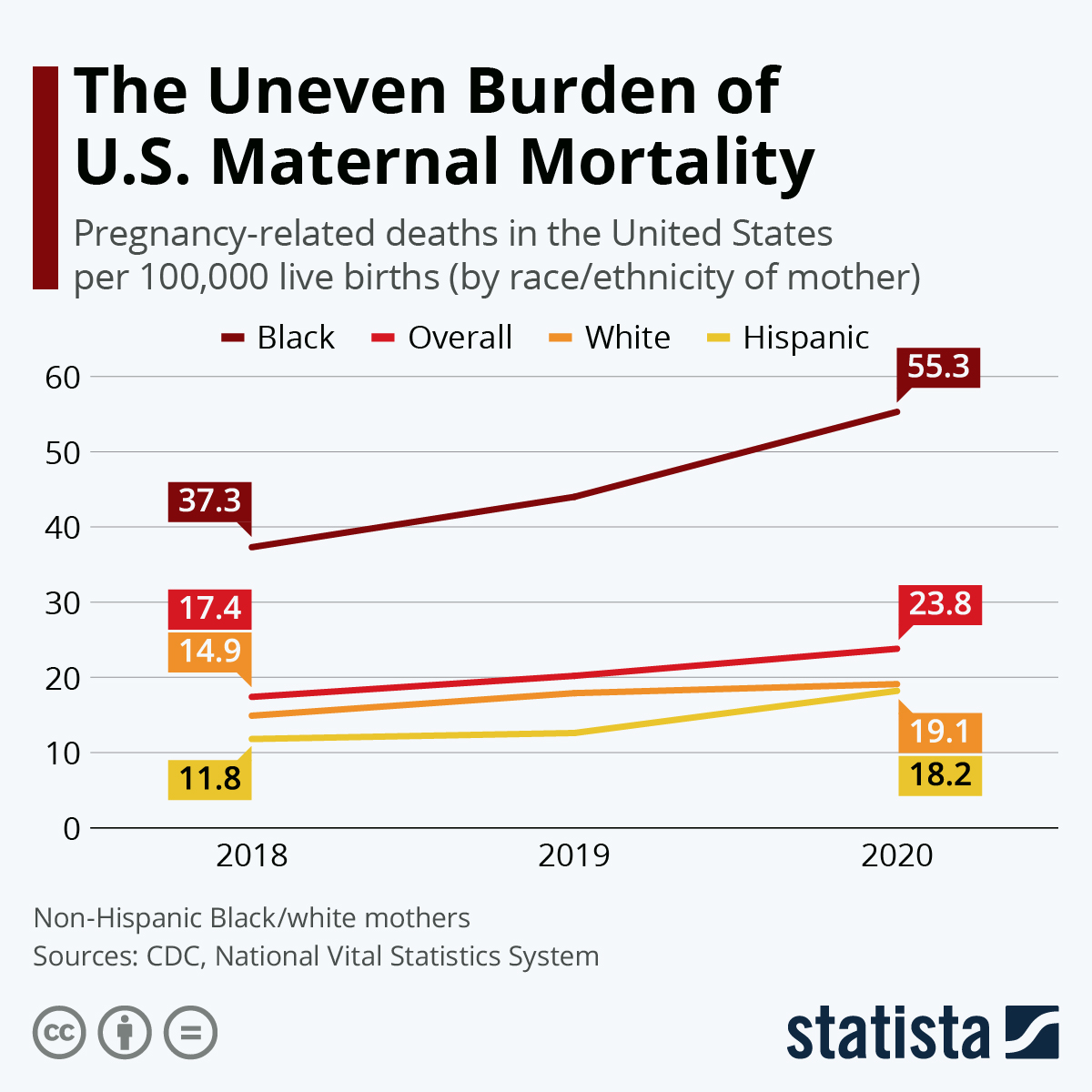
Maternal mortality in the U.S. is a growing concern, especially as pregnancy-related deaths continue to rise amidst alarming health disparities. According to recent studies, over 80% of these deaths are preventable, yet the U.S. remains the leader in maternal mortality rates among high-income nations. The onset of the COVID-19 pandemic in 2020 significantly impacted maternal health, exacerbating existing issues related to inadequate postpartum care and health disparities. Racial and ethnic minorities face the highest risks, with American Indian and Alaska Native women suffering the most severe outcomes. With better policies and healthcare access, we can work towards combating these preventable maternal deaths and improving overall maternal health outcomes across the nation.
The issue of maternal mortality in the United States encompasses a rising trend of pregnancy-related fatalities, calling for immediate attention to maternal health equity. As highlighted in recent analyses, various factors contribute to the stark differences in maternal health outcomes, particularly among diverse racial and ethnic groups. The impact of the COVID-19 pandemic has further complicated the landscape, intensifying challenges surrounding postpartum care and healthcare accessibility. By examining and addressing these critical facets, we can begin to diminish the preventable mortality rates observed in vulnerable populations, ultimately fostering a more equitable healthcare system for all expectant mothers. Understanding the nuances of maternal risk factors and healthcare delivery will be essential in turning the tide on this pressing public health issue.
The Rising Concern of Maternal Mortality in the U.S.
Maternal mortality in the U.S. has reached alarming rates, consistently surpassing those of other high-income countries. Recent studies indicate that over 80 percent of pregnancy-related deaths are preventable, highlighting a critical need for interventions and improved healthcare strategies. This issue is exacerbated by significant disparities that vary by state, race, and ethnicity, with American Indian and Alaska Native women facing the highest mortality rates. The continuous rise in these statistics calls for urgent attention from policymakers and healthcare leaders.
The root causes of this rising maternal mortality rate are multifaceted, influenced by a fragmented healthcare system and inequitable policies that fail to provide adequate prenatal and postpartum care. Women in the U.S. are increasingly affected by chronic health issues, such as hypertension, which plays a significant role in pregnancy-related deaths. Addressing these disparities and improving maternal health outcomes must be a priority in national health discussions.
Understanding Pregnancy-Related Deaths and Their Causes
The U.S. has witnessed a concerning shift in the leading causes of pregnancy-related deaths over the years, with cardiovascular diseases now accounting for over 20 percent of these fatalities. This transition raises critical questions about women’s health, particularly as it relates to chronic conditions like hypertension and pre-eclampsia, which have become more prevalent even among younger women. It’s vital for both healthcare providers and communities to understand the dynamics of these health risks in order to design effective prevention strategies.
Moreover, the rising rates of preventable maternal deaths underscore the importance of quality maternal healthcare. Racial and ethnic disparities persistently contribute to unequal outcomes, suggesting that specific groups face heightened risks during pregnancy and the postpartum period. Analyzing these patterns can guide healthcare systems in creating targeted responses to better serve maternal populations, thus reducing mortality rates overall.
The Impact of COVID-19 on Maternal Health Disparities
The COVID-19 pandemic has had profound implications for maternal health, exacerbating already existing disparities that affect pregnancy-related outcomes. The spike in maternal mortality rates during 2021, a critical year marked by the pandemic, reflects the intersection of healthcare access and systemic inequalities. Evidence suggests that women from marginalized communities were disproportionately affected, revealing deeper structural issues within the healthcare system that need urgent reform.
As we assess the pandemic’s impact, it becomes clear that the need for comprehensive and equitable maternal healthcare systems is more critical than ever. This necessitates the implementation of accessible prenatal and postpartum care programs designed to support all women, particularly those in communities most affected by the pandemic. Effective policy changes and healthcare practices should prioritize stability and accessibility to reduce the extent of preventable maternal deaths in a post-COVID landscape.
Postpartum Care: A Critical Component in Preventing Maternal Mortality
Postpartum care often receives less attention in maternal health discussions, yet it plays a crucial role in reducing maternal mortality. Approximately one-third of maternal deaths occur after the traditional 42-day postpartum period, emphasizing the need for continued healthcare support during this time. The U.S. healthcare system should adapt to recognize that the recovery phase extends beyond a few weeks, allowing for comprehensive care that supports new mothers in their transition.
Investing in extended postpartum programs can significantly mitigate risks associated with late maternal deaths. This includes ensuring access to physical and mental health resources, patient education, and regular follow-ups. By fostering a healthcare environment that prioritizes long-term maternal well-being, we can potentially address the vast disparities currently seen in maternal health outcomes.
Challenges in Tracking Maternal Deaths in the U.S.
One of the significant challenges in mitigating maternal mortality rates in the United States is the lack of a cohesive tracking system for maternal deaths until relatively recently. In 2018, the implementation of pregnancy checkboxes on death certificates enabled better data collection, but considerable gaps remain. A thorough understanding of the specific circumstances surrounding maternal deaths is crucial for developing targeted interventions.
Improving data collection and tracking methods is essential for identifying trends and understanding the multifactorial nature of maternal deaths. As it stands, many states still lack proper systems to adequately analyze data, which hampers the effectiveness of public health initiatives aimed at reducing pregnancy-related fatalities. A robust framework must be established to ensure comprehensive monitoring of maternal health outcomes across the nation.
Addressing Racial Inequities in Maternal Health
The stark racial disparities in maternal mortality rates in the U.S. are troubling, with American Indian, Alaska Native, and Black women facing substantially higher risks compared to their white counterparts. Systemic racism and biases within healthcare delivery contribute significantly to these inequities, indicating a need for healthcare reforms that prioritize diversity and inclusivity in maternal health services. It is imperative that healthcare professionals recognize these disparities and take action to address them by honing in on culturally competent care.
In addition to policy changes, community engagement and advocacy play pivotal roles in curbing racial disparities in maternal health. Empowering marginalized communities with education, resources, and support can bridge the gaps that have persisted for generations. By focusing on both prevention and education, we can begin to create a more equitable healthcare system that effectively reduces the risk of maternal deaths across diverse populations.
Innovative Solutions for Improving Maternal Care
To combat the rising rates of maternal mortality, there is an urgent need for innovative solutions that address the complexities of maternal health. This includes funding programs that provide comprehensive prenatal and postpartum care, utilizing technology to improve access to healthcare information and services, and developing interventions tailored to high-risk populations. Both private and public sectors must collaborate to implement these solutions effectively.
Furthermore, integrating mental health support into maternal care programs can significantly enhance outcomes for mothers, particularly in recognizing and addressing postpartum depression or anxiety. Holistic health approaches are essential in ensuring that all aspects of a woman’s health are considered during and after pregnancy, thereby reducing the risk of preventable maternal deaths as well as improving long-term health outcomes.
The Role of Policy in Maternal Health Improvement
Addressing maternal mortality in the U.S. requires a robust policy framework that prioritizes maternal health at all levels. Policymakers must address the underlying determinants of health disparities by creating laws and policies that ensure equitable access to maternal healthcare services, regardless of an individual’s geographic or socioeconomic status. This includes expanding insurance coverage and access to necessary resources.
Moreover, investing in public health infrastructure is critical for tracking maternal health data and identifying trends that can inform better care practices. Continuous funding and support for maternal health initiatives are crucial to reversing the current trends of increasing maternal mortality rates. By putting maternal health on the legislative agenda, we can promote a nationwide commitment to enhancing care systems and ultimately saving lives.
Community Involvement in Maternal Health Advocacy
Community involvement and advocacy are vital for effecting change in maternal health outcomes. Local organizations can play a significant role by providing education, support, and resources for expectant and new mothers in their communities. By empowering women with knowledge about their health, available services, and potential risks, communities can help reduce preventable maternal deaths.
Furthermore, collaboration between healthcare professionals and community leaders fosters a more holistic approach to maternal health. Engaging with those directly affected by maternal health disparities ensures that solutions are not only evidence-based but also pragmatic and relevant to the communities they are designed to serve. As community efforts grow, they can complement policy initiatives aimed at improving maternal care and health equity.
Frequently Asked Questions
What are the main causes of maternal mortality in the U.S.?
The main causes of maternal mortality in the U.S. are chronic health conditions, particularly cardiovascular disease, which accounts for over 20% of pregnancy-related deaths. Other significant factors include hemorrhage and complications from pre-eclampsia and eclampsia. The rise in obesity and chronic conditions such as hypertension among younger women is also contributing to higher rates of maternal mortality.
How do maternal health disparities impact pregnancy-related deaths in the U.S.?
Maternal health disparities significantly affect pregnancy-related deaths in the U.S., especially among racial and ethnic groups. For instance, American Indian and Alaska Native women experience a maternal mortality rate nearly four times higher than that of white women. These disparities highlight the need for targeted interventions and policy changes to improve maternal health outcomes and access to quality care for all groups.
What is the impact of COVID-19 on maternal mortality rates in the U.S.?
The COVID-19 pandemic has exacerbated maternal mortality rates in the U.S., with a marked increase in pregnancy-related deaths during 2021 as the pandemic began. Factors such as increased barriers to accessing healthcare and the added stresses of the health crisis have contributed to these rising rates, underscoring the need for improved maternal health support during and after the pandemic.
What percentage of pregnancy-related deaths are preventable in the U.S.?
In the U.S., more than 80% of pregnancy-related deaths are considered preventable. This indicates a critical gap in the healthcare system that, if addressed through better prenatal and postpartum care, could significantly reduce maternal mortality rates.
Why is extended postpartum care important for reducing maternal mortality?
Extended postpartum care is crucial because a significant number of pregnancy-related deaths, nearly one-third, occur between 42 days to one year after childbirth. This highlights the need for continuous monitoring and support for new mothers beyond the traditional six-week postpartum visit to ensure better health outcomes.
What role does public health infrastructure play in addressing maternal mortality in the U.S.?
Public health infrastructure plays a vital role in tracking and addressing maternal mortality rates. Continued investment in this infrastructure is necessary to gather accurate data, implement effective healthcare policies, and advocate for better maternal health services, ultimately improving pregnancy outcomes across the nation.
What can be done to address the rising rates of maternal mortality in the U.S.?
To address rising rates of maternal mortality, the U.S. must invest in quality prenatal and extended postpartum care, enhance public health initiatives, and address systemic health disparities across states. Additionally, focusing on education and access to healthcare for at-risk populations can help reduce preventable maternal deaths.
| Key Points | Details |
|---|---|
| Pregnancy-related deaths continue to rise in the U.S. | Over 80% of these deaths are preventable. |
| Highest maternal mortality rate among high-income countries. | Rates have risen from 25.3 per 100,000 live births in 2018 to 32.6 in 2022. |
| Significant racial and ethnic disparities. | American Indian and Alaska Native women had the highest rates at 106.3 per 100,000 live births. |
| Major causes include cardiovascular disease and chronic health conditions. | Cardiovascular disease accounts for over 20% of deaths. |
| Challenge in tracking deaths due to inconsistent data system. | Full implementation of death certificates began in 2018. |
| Need for better healthcare systems during postpartum. | Late maternal deaths make up nearly a third but often go untracked. |
| Investment in public health infrastructure is crucial. | Increasing funding is necessary to improve maternal health outcomes. |
Summary
Maternal mortality in the US continues to rise, highlighting a significant public health crisis that requires urgent attention. Despite the preventability of over 80% of these deaths, the United States holds the highest maternal mortality rate among high-income nations. Disparities based on race and state further complicate the issue, with American Indian and Alaska Native women experiencing the highest rates. The shift in leading causes of pregnancy-related deaths toward chronic health conditions, particularly cardiovascular diseases, signals the need for comprehensive care that extends beyond the immediate postpartum period. Addressing these challenges through improved healthcare infrastructure and targeted policies is essential for reversing the alarming trend in maternal mortality.