AI brain cancer prediction is revolutionizing the landscape of pediatric oncology by offering new hope for early detection and management of cancer recurrence. Recent advancements in artificial intelligence enable more precise predictions, particularly for children diagnosed with brain tumors such as pediatric gliomas. Unlike traditional methods, AI leverages temporal learning to analyze sequential MRI scans, greatly enhancing the accuracy of recurrence predictions and reducing the burden of frequent imaging on young patients. By focusing on delivering personalized care, the integration of AI in medicine is paving the way for innovative strategies that prioritize early intervention and tailored treatment plans. As researchers continue to refine these predictive models, the future for managing pediatric brain cancer looks increasingly optimistic.
The application of artificial intelligence in forecasting brain cancer outcomes represents a significant breakthrough in treating childhood cancers. In recent studies, AI has shown remarkable potential in enhancing cancer recurrence prediction, particularly concerning gliomas found in pediatric patients. By employing advanced analytical techniques, like temporal learning, these intelligent systems can assess multiple imaging results to provide better insights into a patient’s condition over time. This approach not only mitigates the stress associated with repeated imaging procedures but also aligns with the broader movement to harness technology for enhanced medical imaging in childhood cancer treatment. As AI becomes an integral part of pediatric cancer imaging, it promises to facilitate more effective monitoring and intervention protocols.
The Role of AI in Pediatric Cancer Imaging
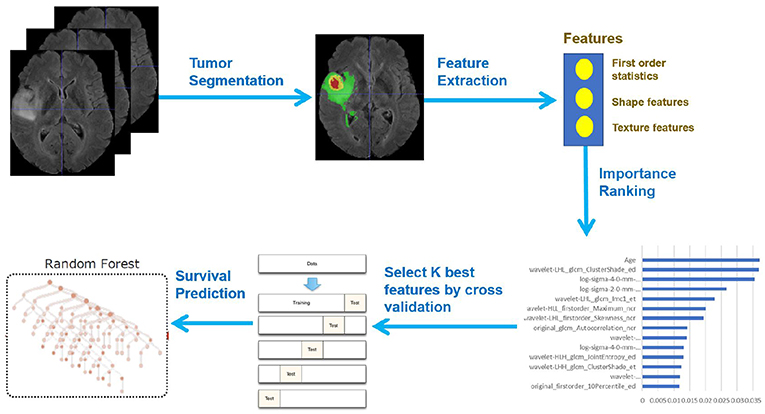
Advancements in artificial intelligence (AI) are reshaping our approach to pediatric cancer treatment, particularly in imaging diagnostics. AI technologies, particularly those utilized in pediatric cancer imaging, enable healthcare professionals to analyze a vast amount of data quickly and accurately. Machine learning algorithms are being trained to detect anomalies in MRI scans that may signal a recurrence of gliomas, a common type of brain tumor in children. This integration of technology into medicine not only enhances diagnostic capabilities but also allows for timely interventions, significantly improving patients’ prognosis.
AI in medical imaging leverages complex algorithms to support oncologists in identifying patterns and changes over time. In pediatric glioma cases, traditional imaging methods often rely on radiologists’ interpretations of single scans, which can lead to missed subtle indicators of tumor recurrence. The use of AI tools that focus on iterative scan analysis allows for a comprehensive overview, providing physicians with a detailed timeline of tumor behavior. Consequently, healthcare providers can develop tailored treatment plans, ultimately benefiting the young patients who undergo this rigorous process.
AI Brain Cancer Prediction: A Breakthrough in Relapse Risk Assessment
The recent Harvard study highlighting AI brain cancer prediction marks a significant advancement in the fight against pediatric gliomas. By employing a unique temporal learning technique, the AI tool surpassed traditional methods in predicting relapse risks, boasting an impressive accuracy of 75-89 percent. Traditional methods had only achieved around 50 percent accuracy, which proves to be far less effective. This advancement is critical as it allows for better identification of at-risk patients—vital information that can shape treatment strategies and improve survival outcomes.
The AI model’s reliance on multiple MRI scans taken over time presents an innovative approach to cancer recurrence prediction. Unlike standard practices queuing single imaging analysis, this methodology understands the progression of the disease through a series of scans. The significance of this leap in capability cannot be understated; it offers oncologists the chance to intervene earlier in the treatment process avoiding potentially devastating outcomes. As we examine the implications of improved AI brain cancer prediction methods, we see a promising pathway toward more personalized medicine in pediatric oncology.
Understanding Temporal Learning in Medical Imaging
Temporal learning represents a pioneering concept in medical imaging, fundamentally altering how AI interprets MRI scans. By synthesizing data from sequences of scans over time, rather than relying on isolated images, researchers have developed models that more accurately reflect the dynamics of brain tumors like pediatric gliomas. This approach not only identifies current states of the tumors but also anticipates future challenges in patient care, making it a crucial tool in the oncology toolkit.
The significance of temporal learning lies in its ability to recognize subtle changes in tumor behavior that might otherwise go unnoticed in single-scan analyses. It offers insights into how gliomas evolve post-surgery, allowing for timely adjustments in treatment protocols. As further research and clinical validation are underway, the potential applications of temporal learning in pediatric cancer imaging could extend beyond gliomas to other types of cancers, paving the way for more nuanced, effective treatment approaches.
Improving Predictions of Cancer Recurrence in Pediatric Gliomas
One of the chief challenges in treating pediatric gliomas is predicting the likelihood of recurrence after initial treatment. Traditional models have struggled with this due to their reliance on static imaging interpretations which often overlook crucial temporal changes. Researchers are now incorporating innovative AI systems that utilize a variety of consecutive scans. This new paradigm enhances predictive models leading to a better understanding and management of the complexities surrounding glioma recurrences.
With improved accuracy of AI in predicting cancer recurrence, families can find a greater sense of security and clarity in treatment plans. As oncologists can better identify high-risk patients, they will be able to customize care strategies, mitigating the risk while maximizing the potential for successful outcomes. This evolution in predictive capability represents a significant leap in pediatric oncology, promising hopeful advancements for children battling brain cancer.
Future Implications of AI-Driven Medical Techniques
As AI technology continues to evolve, its impact on medical practices—especially in oncology—will undoubtedly expand. The promising results from studies demonstrating AI’s efficacy in pediatric glioma prediction suggest potential applications in various other aspects of healthcare. From optimizing imaging processes to enhancing patient monitoring, the future of AI in medicine is bright. The anticipated developments in AI will undoubtedly help enhance efficiencies, reduce costs, and ultimately lead to better health outcomes for patients.
Moreover, the growing collaboration between hospitals and research institutions signifies a collective commitment to pioneering AI applications in pediatric oncology. Future clinical trials aiming to test AI-informed risk predictions can directly translate into practical treatment adjustments, thereby paving the way for a new era in pediatric cancer care. As these technologies become integrated into everyday practices, the outlook for young patients grappling with cancer recurrence is promising, echoed in a hopeful expectation for improved survival rates.
The Importance of Institutional Collaboration in Cancer Research
Institutional collaboration is vital for the advancement of cancer research, particularly in the context of pediatric gliomas where resources and expertise can be pooled to tackle complex challenges. Studies conducted by institutions like Mass General Brigham, Boston Children’s Hospital, and Dana-Farber/Boston Children’s highlight the power of collective innovation in AI-based medical research. Such partnerships enable researchers to harness a broader range of MRI data, driving the quest for precise diagnostic tools and predictive models.
Collaborative efforts not only enhance the quality of research but also facilitate the sharing of best practices and resources, which is crucial when it comes to validating the efficacy of AI applications in medicine. By aligning their goals and expertise, these institutions lay the groundwork for significant advancements in early detection and treatment options for pediatric cancer patients. Such teamwork ultimately fosters an environment where innovative solutions can flourish, magnifying the potential impacts on patient care.
Addressing Psychological Burdens in Pediatric Cancer Patients
Beyond the physical and medical challenges of pediatric brain cancer, the psychological toll on young patients and their families is noteworthy. Frequent imaging and monitoring can lead to anxiety and stress, compounding the already delicate emotional state that comes with a cancer diagnosis. Addressing this psychological burden is as integral as the technical advancements offered by AI, as a holistic approach to treatment must consider the mental health of patients.
Integrating AI tools that reduce the frequency of unnecessary imaging for low-risk patients could alleviate some of this stress. This empowers families to focus on healing rather than enduring the anxiety of repeated scans without clear necessity. As research progresses with AI making strides in accurately predicting recurrence, families can gain confidence in their treatment avenues. Mental well-being, alongside medical advancements, must be prioritized to ensure that comprehensive care frameworks are established for pediatric glioma patients.
The Future of Pediatric Oncology: A Synergy of AI and Human Expertise
The fusion of AI technology with human expertise represents the frontier of pediatric oncology. While AI offers enhanced precision in predicting cancer recurrence, the role of healthcare providers remains indispensable. This synergy ensures that while algorithms can highlight risks and inform treatment pathways, the compassion and judgment of medical professionals guide these decisions. AI can augment decision-making processes, but it cannot replace the empathy and intuition that healthcare professionals bring to patient interactions.
As we look towards the future, training new generations of oncologists to embrace and effectively integrate AI tools within their practices will be crucial. Educational initiatives are needed to equip clinicians with the knowledge to interpret AI outputs while maintaining their focus on patient-centered care. Together, humans and machines can revolutionize pediatric cancer treatment by optimizing diagnoses, personalizing care, and ultimately enhancing outcomes for children battling conditions like gliomas.
Frequently Asked Questions
How does AI in brain cancer prediction enhance the management of pediatric gliomas?
AI in brain cancer prediction significantly improves the management of pediatric gliomas by accurately analyzing MRI scans over time, allowing for better identification of patients at risk for cancer recurrence. This advanced predictive capability surpasses traditional methods, providing healthcare teams with valuable insights for tailored follow-up care.
What is the role of temporal learning in AI brain cancer prediction for pediatric patients?
Temporal learning plays a crucial role in AI brain cancer prediction by enabling the analysis of multiple MRI scans over time. This technique enhances the model’s ability to detect subtle changes associated with the recurrence of pediatric gliomas, leading to improved prediction accuracy compared to single-scan evaluations.
Why is cancer recurrence prediction important in the treatment of pediatric gliomas?
Cancer recurrence prediction is vital in the treatment of pediatric gliomas because early identification of high-risk patients can improve treatment outcomes and minimize unnecessary follow-ups. AI tools that enable precise risk assessment can significantly reduce the burden on young patients and their families.
What advantages does AI provide over traditional methods in pediatric cancer imaging?
AI provides numerous advantages over traditional methods in pediatric cancer imaging, including higher accuracy in predicting relapse, the ability to process multiple images with temporal learning, and a reduction in the emotional and physical strain of frequent monitoring through advanced predictive analytics.
How does predicting cancer recurrence with AI impact clinical outcomes for pediatric patients?
Predicting cancer recurrence with AI has the potential to enhance clinical outcomes for pediatric patients by initiating timely interventions for those identified as high-risk, thereby personalizing care and potentially decreasing the overall treatment burden associated with continuous imaging.
Can AI brain cancer prediction change the approach to follow-up care in pediatric glioma patients?
Yes, AI brain cancer prediction can dramatically change the approach to follow-up care in pediatric glioma patients by enabling more focused monitoring. High-risk patients may receive more intensive care, while low-risk patients may have reduced follow-up requirements, leading to better use of medical resources.
What is the significance of the findings from the recent study on AI and pediatric gliomas?
The findings from the recent study on AI and pediatric gliomas are significant as they demonstrate that AI can predict recurrence with 75-89% accuracy through temporal learning, showcasing its potential to transform ongoing monitoring practices and improve treatment strategies within pediatric oncology.
What are the future implications of AI in medicine for children with brain cancer?
The future implications of AI in medicine for children with brain cancer include the possibility of improved early detection of recurrence, personalized treatment plans based on precise risk assessments, and an overall shift towards more effective and less invasive management options in pediatric oncology.
How does analyzing multiple MRI scans contribute to AI brain cancer prediction?
Analyzing multiple MRI scans contributes to AI brain cancer prediction by allowing the model to track subtle changes over time that would otherwise be missed in singular scans. This comprehensive view enables a more accurate prediction of relapse for children with gliomas.
What steps are necessary for the clinical application of AI tools in estimating cancer recurrence risk?
For the clinical application of AI tools in estimating cancer recurrence risk, further validation across diverse clinical settings is necessary. This includes conducting clinical trials to assess whether AI-driven predictions can lead to improved patient outcomes and optimized follow-up strategies.
| Key Points |
|---|
| AI performs better than traditional methods in predicting brain cancer relapse risk. |
| Study conducted at Mass General Brigham and Boston Children’s Hospital. |
| AI tool analyzed nearly 4,000 MRI scans from 715 pediatric patients. |
| Temporal learning technique trains AI using multiple scans over time. |
| Prediction accuracy improved to 75-89% using multiple scans compared to 50% with single scans. |
| Need for further validation before clinical application of AI predictions. |
| Potential benefits of reduced imaging frequency and targeted therapies for high-risk patients. |
Summary
AI brain cancer prediction has emerged as a leading-edge solution in the early detection of relapse in pediatric patients with gliomas. The enhanced accuracy provided by AI tools over traditional methods not only offers hope for improved patient outcomes but also alleviates the stress associated with frequent medical imaging. This innovative approach underscores the potential for AI to revolutionize cancer care, particularly in vulnerable populations. As ongoing studies pave the way for clinical trials, the integration of AI in monitoring pediatric brain cancer patients could transform the landscape of oncological treatment strategies.